Family Medicine Residency
Shasta Community Health Center in Redding, California sponsors an accredited Rural Training Program in Family Medicine affiliated with the University of California at Davis. The program provides strong exposure to obstetrics, pediatrics, procedures, and homeless/community medicine. Three residents per year (PGY-1 through PGY-3) are accepted in each class. The SCHC Family Medicine Residency works closely with the Mercy Redding Family Practice Residency Program, rotating on inpatient services and sharing call. Outpatient continuity clinics are done at SCHC sites.
Our goal is to train full spectrum family practice physicians to practice in a Community Health Center environment serving the otherwise medically underserved. The faculty at the SCHC Family Medicine Residency strive to create the next generation of caring, dedicated health care providers.

Message from the
Program Director
We look forward to working with you and teaching our residents full spectrum Family Medicine in a small community with an underserved population. Redding is located in beautiful Northern California and offers an abundance of outdoor activities and recreational opportunities. Our city has many of the amenities found in larger cities. Shasta Community Health Center provides a supportive and compassionate training staff. We look forward to discussing this new and exciting opportunity with you.
Sincerely,
Debra Lupeika, MD
For more information about this exciting Resident Program opportunity, you can email schcresidency@shastahealth.org, or you can call (530) 246-5951.

Meet Our Leadership and Faculty











Meet Our Residents








Our Curriculum and Rotations
Enjoy the Benefits of Residency at SCHC

Compensation (House Staff Salaries 2023-2024)
- PG-I $64,480 per year
- PG-II $68,349 per year
- PG-III $73,798 per year
Other Benefits
- Health/Dental/Vision plans
- All meals while on duty (daytime as well as when on call)
- Lab Coats provided
- Sick leave
- Four weeks vacation per year
- Book allowance- $300
- Free parking
- AAFP membership
- DEA licensure
- Medical licensure
- UpToDate access
- Epocrates
- ABFM Board Exam- paid if taken during PG-III
- Moving allowance- $1,000
- Pediatric ER Stipend
- YMCA Members
- AMA Membership
- NVMA Membership
- Calm App
Rotation Locations
Mercy Medical Center in Redding is the primary inpatient teaching location for rotations in medicine, pediatrics, and obstetrics. Our residents participate in hospital call, lectures, and rounds with our sister program Mercy Redding Family Medicine Residency.
SCHC residents have hands-on experience during the surgery rotation at Shasta Regional Medical Center. Further obstetric experience is available at St. Elizabeth's Hospital in nearby Red Bluff for residents wishing additional training. SCHC residents enjoy a supportive and educational experience in all of these affiliated hospitals.
SCHC Family Practice residents also spend dedicated time in Pediatric Emergency Medicine at UC Davis Medical Center in Sacramento – giving residents experience in pediatric emergencies and urgencies.
Our program is designated as a Rural Prime Program through UC Davis. First year residents will spend four weeks at a rural clinic location, and can return for more rural clinic exposure during the second and third years as they wish during elective blocks. SCHC rural sites are within 20 minutes of the residency center, and others are more remote and residents will lodge in that area during the rotation.
Learning Resources & Rotation Information
Learning Resources is a collection of useful information and materials for the Shasta Health Residents. It contains documents and links related to various rotation topics, such as cardiology, emergency medicine, geriatrics, etc. You can use this resource to review the learning objectives, expectations, and evaluation methods for each rotation. You can also access relevant articles, guidelines, and websites to enhance your knowledge and skills.

Advocacy and Scholarly Activity
Advocacy and scholarly activity are integral components of the SCHC Residency program. Residents are encouraged to participate in various projects and initiatives that aim to improve the health and well-being of the community. Residents also have the opportunity to conduct research, present their findings at local and national conferences, and publish their work in peer-reviewed journals. The program provides mentorship, support, and resources to help residents develop their skills and interests in these areas.
Street Medicine / MAT
Residents rotate into dedicated experiences in homeless and community medicine. Pain management, addiction medicine, infectious diseases, palliative care, and public health are all emphasized. This is the forte experience of this training program. All residents are expected to obtain their DEA: X-waiver upon licensure to facilitate participation in the Medically Assisted Therapy (MAT) clinic in Residency. This experience prepares our residents to treat addiction involving opiates, stimulants, tobacco, alcohol and other substances.
We believe in advocating for the underserved and homeless in our community. Our CEO and one of our residents travel annually to Washington, D.C. to meet with senators, congressmen and staffers to further the cause of underserved care. Residents and faculty attend the annual National Health Care for the Homeless Council conference. Rural rotations strengthen this training experience, allowing the family practice resident to understand and gain ability with a variety of healthcare systems and diverse patient populations.
Project HOPE is a designated mobile and street medicine outreach program of SCHC. Health Outreach for People Everywhere supplies medical care via EMR integrated mobile units in the homeless community. Weekly street medicine outreach teams contact our homeless in their camps and on the street. We collaborate with our community to work toward a continuum of care for our most vulnerable populations.
Medical Services
- Examinations and immunizations
- Preventative healthcare
- Treatment of acute illness or injury
- Management of chronic diseases
- Diagnosis and treatment of sexually transmitted infections
- Medically Assisted Therapy
Special Services
We provide additional services to meet the special needs of our target populations:
- Developmentally Disabled
- Children
- Homebound
- Homeless or those at risk of homelessness
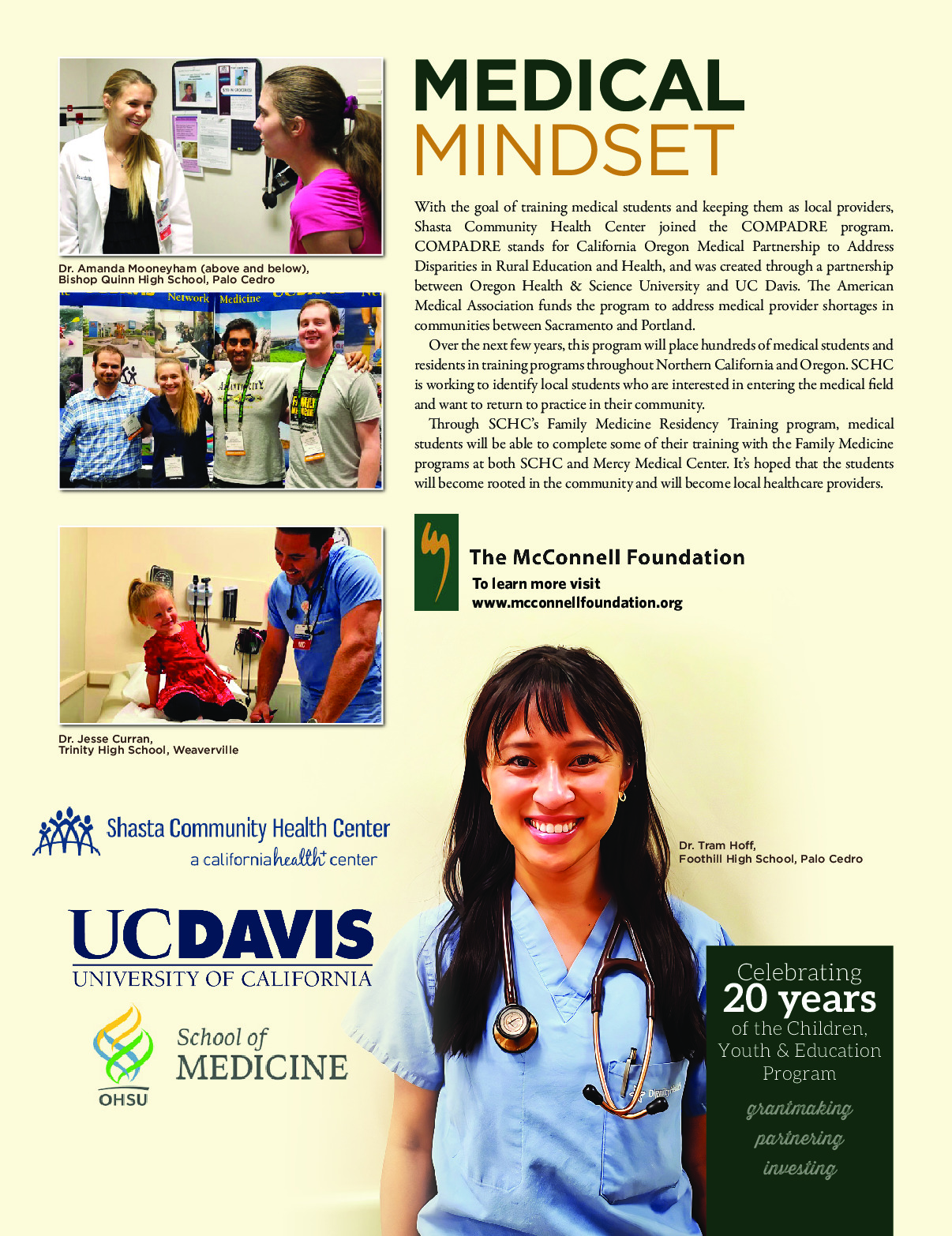
The COMPADRE Program
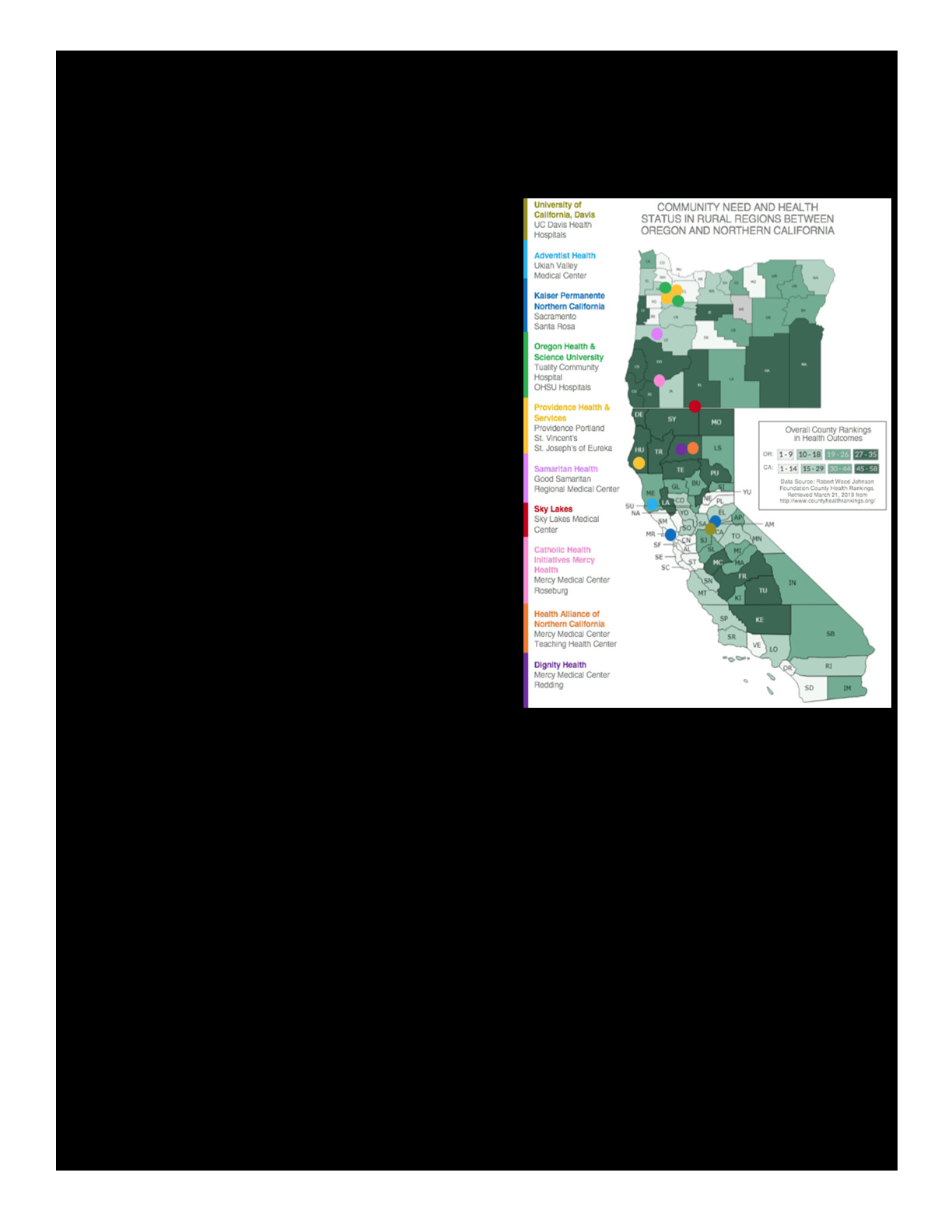
California Oregon Medical Partnership to Address Disparities in Rural Education and Health (COMPADRE) is a multifaceted program that aims to reduce health disparities by transforming the physician workforce – to be better prepared, more equitably distributed and more deeply connected to underserved communities.
More specifically, COMPADRE will:
- Fundamentally change how learners are selected into UME and GME
- Redesign the UME to GME transition so learners gain first-hand experience in their future clinical learning environments
- Better prepare residents to care for populations in under-resourced settings
- Enhance well-being by nurturing meaningful longitudinal relationships within a thriving learning community
- Reduce regional health disparities.
If you are a student with an interest in rural medicine, specifically Northern California or Oregon, please contact us for further information about this innovative program. Selected candidates will have the opportunity to move more directly and efficiently from college /university to medical school and to residency.